6 Questions: What’s It Like To Work In Anesthesiology?
By Hadiyah Brendel
 |
| Army Lt. Col. (Dr.) Robert Vietor (Photo credit: Tom Balfour, USU) |
Physician: Army Lt. Col. (Dr.) Robert Vietor
Title: Anesthesiology Clerkship Director, Vice-Chair of Anesthesia, F. Hébert School of Medicine, Uniformed Services University (USU)
Years in Anesthesiology: 8 years
Special Interests: Regional anesthesia, pain medicine, operational anesthesia or anesthesia in austere environments
Favorite Accolade: San Antonio Uniformed Services Health Education Consortium (SAUSHEC) Best Anesthesia Research Resident Award.
Q. Why did you decide to specialize in Anesthesiology?
A. When I was young, I always wanted to be a doctor. I had my appendix out when I was 15, so at that point, I decided I wanted to be a surgeon. I thought it was really cool that he was able to take me from being really sick to healthy again. Almost overnight. Then when I did my surgery clerkship as a USU student, I realized I don’t really have the personality for surgery. Surgery attendings told me I smile too much, I’m too happy to be a surgeon. I knew I still loved the O.R. I liked taking care of critically ill patients. So I started looking toward anesthesia. I enjoyed the real-time applications of physiology and pharmacology. And I enjoyed the fact that when we’re caring for patients, and making intervention, we see that impact immediately. I don’t have to wait and see what’s going to happen, because it happened. At that point I said, this is more my personality, more my specialty.
Q. What does an Anesthesiologist do?
A. We typically guide patients through the entire peri-operative experience. That’s what a lot of people don’t realize. We see them before surgery to verify their optimized and essentially ready for surgery. During surgery, we try to keep them comfortable and physiologically normal. Our goal is to maintain everything in equilibrium. After surgery, we typically monitor patients in the PACU (post-anesthesia care unit) or ICU. We make sure they’re still comfortable from the surgery, as well as make sure they’re recovering appropriately both cognitively and physiologically.
In addition, we also take care of patients on labor and delivery. We do epidurals and get to be a part of that world too. I really enjoy that. We also respond to all in-hospital emergencies. So it’s a wide variety of activities we get to participate in which makes it kind of fun.
Q. What is one of the biggest challenges about working in this field?
A. I think one of the hardest things about anesthesia is staying vigilant when everything is going well. I always tell
stories about a young healthy person coming in for a routine procedure and it’s easy to say, “This is going to be easy. Chip shot. I don’t really need to pay that much attention,” when in reality, that’s when bad things happen.
They say anesthesia is 90% boredom and 10% sheer terror. I don’t think that’s true. I find the 90% boring to be incredibly exciting. You’re constantly making decisions and moving. I would say there’s never a boring moment in anesthesia. And for the most part, when things aren’t going well, that 10% they speak of, we’ve been trained for that. That’s why we’re there. So I don’t necessarily agree with the 90/10 rule. I think it’s always exciting. I think that 10% – and it’s not as high as 10% – but that 10% just gives us the ability to showcase our expertise.
We have a habit of always looking calm during surgery. So people take that as we’re bored or we’re not doing anything. When in reality, we’re analyzing a lot of data, we’re constantly thinking, making decisions to ensure the patient is moving in the right direction, anticipating those complications that hopefully don’t happen. But sometimes they do.
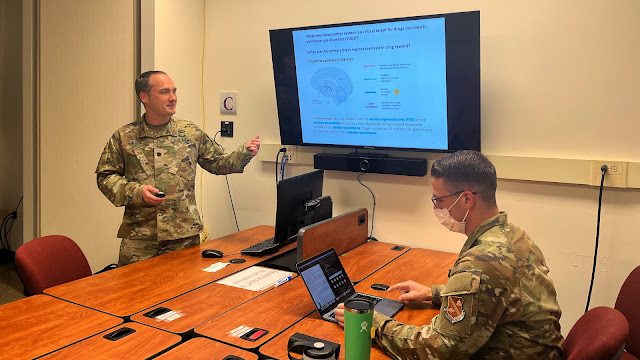 |
| Army Lt. Col. (Dr.) Robert Vietor says "you're constantly making decisions and moving" while working in anesthesiology. (Courtesy photo) |
Q. What aspects of your job do you find most fulfilling?
A. The biggest thing for me is making a difference in people’s lives. Whether it's intubating a patient with respiratory distress in the ICU at Walter Reed, transfusing a wounded soldier in Iraq, or teaching students at USU, I know that the things I do every day and the patients I take care of, I impact their lives. It definitely makes a difference.
It’s nice when you take someone who is critically ill from the ICU to the OR, to take care of the surgical issue they have, and then back to the ICU and then days or weeks later they finally leave the ICU and they go home. You get to see them hugging their families. You feel like you made a difference in your job. And it’s across the entire spectrum, from deployed experiences to stateside experiences, and now I teach the students. To see the students grow and develop, as either military physicians or anesthesiologists, is great; to see how far they’ve come in the years that I’ve been here.
Q. In your medical studies, and as a USU alumnus, what prepared you the most for this profession?
A. The biggest thing for anesthesiologists is we work with every service in the hospital. It’s not enough to just know anesthesia. You have to understand what orthopedic surgery requires, you have to understand what internal medicine requires. We provide services to radiation oncology when they do radiation therapy, we go to interventional radiology when they do their procedures, we do cardiology, pediatric sedation, we go to the ER, the OB deck, ICU, or reproductive endocrinology.
We have to provide anesthesia and sedation for all different people and all different services. And they all have very unique considerations. So the biggest thing for me as a USU student, then an intern, and then a resident at SAUSHEC was learning: you have to know everybody’s job to be good at anesthesia. ‘What does reproductive endocrinology and infertility need from me when we do an egg harvest?’ Or ‘what are the goals of interventional radiology versus some of the other services?’ You’re supporting them. On the Pain service, we sometimes do our own thing. But for the most part, we are a supporting character. We help everybody else do their job.
It’s a very interesting place to be. You’re rarely the star but you’re always playing that supporting role to everyone else.
Q. What advice can you offer medical students considering this specialty?
A. I always tell them, don’t be a stranger. Reach out to us early. We want to engage with them. Traditionally, most students haven’t taken the anesthesia clerkship until late in their medical school training. So by the time they’ve seen it, they’ve already decided to do something else. I’m the perfect example of that. I was dead set on doing general surgery until I experienced surgery and thought, “Oh, I don’t really like this as much as I thought I would. But there’s this other thing that’s kinda like surgery that I can do.” So I try to engage students to just come talk to us, hang out with us in the OR for a day or two. I want to make sure they know the door is open. Ensure they know they can reach out to us, talk to us, spend time with us; for them to learn more about our specialty before it's hard to backtrack and come back to us.
And I love chatting about military anesthesia, or anesthesia, in general. If students say ‘hey, after talking to Dr. Vietor I wanna do family practice’ or ‘I want to do surgery,’ great. I’m happy I was able to help them make that decision. But don't rule out talking to us or getting to know a little about anesthesia. Because I do think that it’s a great specialty. It’s something a lot of students don’t see until later in their training, or later in their career. We have a lot of physicians come back to us after they’ve practiced for a while. Maybe it [their specialty selection] wasn’t the best fit for the rest of their life. There are alot of things that are fun when you first graduate medical school that aren’t as fun when you’re older. I think anesthesia continues to be enjoyable. It’s a good specialty. We really all enjoy everything about it. I want to expose as many students as possible so they can make good decisions when it comes to specialties.





