‘Hack-a-Vent’ Challenge Leads to Innovative, Low-Cost Ventilators
By Sarah Marshall
Amid the global pandemic, hospitals across the country have filled with patients suffering from respiratory distress due to COVID-19. To help keep up with a demand for ventilators, the Department of Defense (DoD) recently launched a collaborative effort across the services, along with the Uniformed Services University (USU), to harness innovation and potentially save lives.
In March, using the U.S. Special Operations Command digital platform, Vulcan, the DoD put out a call for proposals to build domestically-sourced ventilators that would be easy to operate and would cost under $500 to produce. A week after the effort, referred to as the “Hack-a-Vent” challenge, was launched, 172 ventilator proposals were submitted.
“Most of the proposals were truly innovative ventilators,” said Navy Cmdr. (Dr.) Arlene Hudson, chair of Anesthesiology at USU.
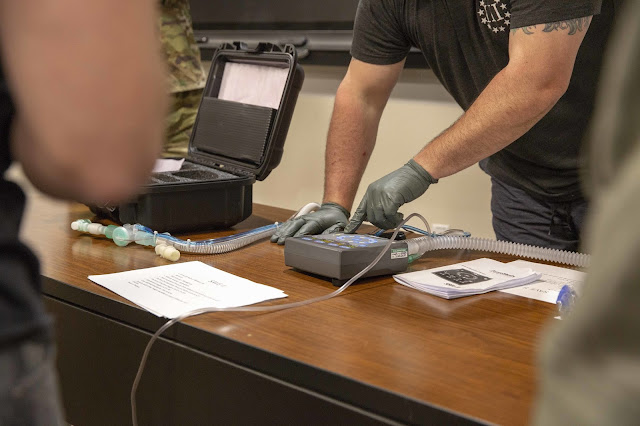
Hudson led a team from USU and Walter Reed National Military Medical Center (WRNMMC) to assess and select the proposals submitted to Vulcan and test the prototypes in a USU lab, testing the ventilators’ ability to control ventilation. The clinical assessment team, made up of surgical, medical, and critical care experts, helped narrow the proposals to five finalists, based on criteria they developed for clinical usability and the most important features that would be required to support the most limited ventilation requirements. Their team also worked with a panel of engineers who tested the basic mechanics of the prototypes, ensuring the technology would be feasible. Five prototypes from organizations spanning large corporations, small businesses, universities and government engineering teams were selected for further development.
Hudson noted the remarkably quick turnaround to garner and develop these prototypes, obtain the necessary research compliance approvals at USU to test them in the lab, and then thoroughly assess their clinical and engineering capabilities. Normally, this process would take years, but instead took only a few weeks due to the ability to leverage an existing large animal lab established for the Battlefield Shock Organ Support program to address this immediate national need.
“It was really an impressive effort. It was really extraordinary,” Hudson said.
The challenge and resulting development process would not have been a success if not for the incredible team effort, according to Hudson. The group included a number of USU faculty, including Army Col. (Dr.) Jessica Bunin, Army Lt. Col. (Dr.) Jacob Collen, Army Lt. Col. (Dr.) Christian Popa, Navy Cmdr. (Dr.) John Benjamin, and Navy Cmdr. (Dr.) Ashley Humphries.
“The success of this effort is a testament to the university’s close ties with Walter Reed, and support from the university’s leadership,” Hudson added. “This could not have been done on a dime. It’s because of the support that already existed for military-relevant research that facilitated and allowed for us to turn this around so quickly. Thanks to this effort, we will fill a gap and potentially save lives.”
Amid the global pandemic, hospitals across the country have filled with patients suffering from respiratory distress due to COVID-19. To help keep up with a demand for ventilators, the Department of Defense (DoD) recently launched a collaborative effort across the services, along with the Uniformed Services University (USU), to harness innovation and potentially save lives.
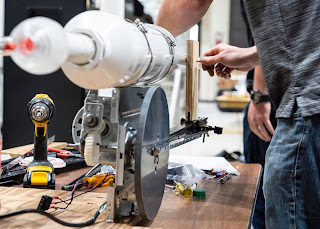 |
| NSWC PCD teams developed ideas and a ventilator prototype in support of the Department of Defense (DoD) Hack-a-Vent Innovation Challenge. (Photo by Eddie Green) |
“Most of the proposals were truly innovative ventilators,” said Navy Cmdr. (Dr.) Arlene Hudson, chair of Anesthesiology at USU.
Hudson led a team from USU and Walter Reed National Military Medical Center (WRNMMC) to assess and select the proposals submitted to Vulcan and test the prototypes in a USU lab, testing the ventilators’ ability to control ventilation. The clinical assessment team, made up of surgical, medical, and critical care experts, helped narrow the proposals to five finalists, based on criteria they developed for clinical usability and the most important features that would be required to support the most limited ventilation requirements. Their team also worked with a panel of engineers who tested the basic mechanics of the prototypes, ensuring the technology would be feasible. Five prototypes from organizations spanning large corporations, small businesses, universities and government engineering teams were selected for further development.
Hudson noted the remarkably quick turnaround to garner and develop these prototypes, obtain the necessary research compliance approvals at USU to test them in the lab, and then thoroughly assess their clinical and engineering capabilities. Normally, this process would take years, but instead took only a few weeks due to the ability to leverage an existing large animal lab established for the Battlefield Shock Organ Support program to address this immediate national need.
“It was really an impressive effort. It was really extraordinary,” Hudson said.
The challenge and resulting development process would not have been a success if not for the incredible team effort, according to Hudson. The group included a number of USU faculty, including Army Col. (Dr.) Jessica Bunin, Army Lt. Col. (Dr.) Jacob Collen, Army Lt. Col. (Dr.) Christian Popa, Navy Cmdr. (Dr.) John Benjamin, and Navy Cmdr. (Dr.) Ashley Humphries.
“The success of this effort is a testament to the university’s close ties with Walter Reed, and support from the university’s leadership,” Hudson added. “This could not have been done on a dime. It’s because of the support that already existed for military-relevant research that facilitated and allowed for us to turn this around so quickly. Thanks to this effort, we will fill a gap and potentially save lives.”