USU Researchers Use Therapeutic Peptides to Develop Skin Substitutes for Wound Healing
By Vivian Mason
Our skin acts as a protective barrier against the external environment to prevent infections and fluid losses. Thus, preserving skin integrity is an essential requirement to staying healthy. When large regions of skin are damaged by burns or lost by trauma, there is a need to cover the wounded area. This can be accomplished by using split-thickness skin grafts or a variety of skin substitutes. These are life-saving interventions, but advances are needed to minimize scarring and form skin with more normal function and appearance.
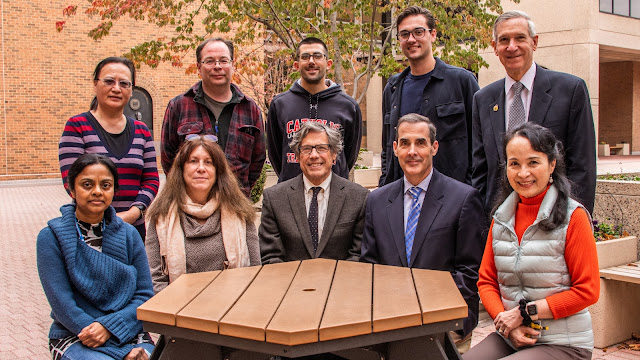
Thomas Darling, M.D., Ph.D., professor and chair in the Department of Dermatology at the Uniformed Services University (USU), is researching skin substitutes.
Says Darling, “We’re developing bioengineered skin substitutes composed of living human cells that are capable of forming hair follicles. These hair follicles produce hair important for appearance. They also have sebaceous glands that produce oils that help lubricate the skin and ward off bacteria. Hair follicles are also repositories of stem cells that are called upon for regeneration of skin structures.”
A major challenge for the next-generation skin substitute is ensuring robust hair follicle formation. Investigators are testing different compounds that may enhance the ability of human cells to form hair follicles.
In 2018, Dr. Darling’s search for compounds that promote hair follicle formation led him to a seminar series sponsored by the Transforming Technology for the Warfighter (TTW) program. The TTW program is currently led by Army Col. Chad Black, director of USU’s Biomedical Instrumentation Center.
Speakers from universities in Boston presented potential opportunities for collaboration, including descriptions of a set of novel peptides identified by Ira Herman, Ph.D., professor and director emeritus of the graduate program in cell, molecular, and developmental biology in the Tufts Center for Innovations in Wound Healing Research at Tufts University School of Medicine. The Tufts peptides had properties that Dr. Darling thought would be useful for skin substitutes.
According to Herman, “We identified specific bioactive peptides that are produced from collagenase treatment of the extracellular matrix that stimulate the healing process within a wound. By creating combinations of several key peptide fragments, we are able to synthesize an entirely novel class of wound-healing peptides that promote the fundamental response to injury, blood vessel formation, and epithelialization.”
Drs. Darling and Herman obtained funding from the TTW program, allowing them to test the Tufts peptides in skin
substitutes.
“For these experiments,” notes Darling, “we used human cells that divided several times in culture, as would be needed to generate enough cells to cover a large skin defect. As expected based on the work of others, we found that skin substitutes using these cells had a reduced capacity to form hair follicles. We are now testing whether the presence of bioactive peptide during creation of the skin substitute restores capacity for hair follicle formation.”
Positive preliminary results of peptides on skin substitutes has led to new initiatives by Drs. Darling and Herman.
One initiative is to incorporate Tufts peptides into bioprinted human skin through collaboration with Dr. George Klarmann and investigators in USU’s Center for Biotechnology (4D Bio3).
4D Bio3 explores and adapts promising biotechnologies for the warfighter.
Another initiative, through collaborations with Dr. Regina Day in USU’s Department of Pharmacology and Molecular Therapeutics and Dr. Juliann Kiang at USU’s Armed Forces Radiobiology Research Institute, is to test the effects of peptides on mitigation of radiation burns and combined radiation and skin wounds.
The last initiative involves Dr. Kristo Nuutila at the U.S. Army Institute of Surgical Research to test the effects of peptides on full-thickness wounds and burns.
“Confirmation that these peptides could act synergistically to improve human wound healing moves our research one significant step closer to clinical application,” acknowledges Herman. “We hope that these discoveries and new technologies will have broad implications for more rapid healing and improved skin regeneration of wounds that are acute or chronic, or caused by trauma, radiation, or thermal injury.”